IL-3 Reporter HEK 293 Cells
| Product | Unit size | Cat. code | Docs. | Qty. | Price | |
|---|---|---|---|---|---|---|
|
HEK-Blue™ IL-3 Cells Human IL-3 Reporter Cells |
Show product |
3-7 x 10e6 cells |
hkb-il3
|
|||
|
HEK-Blue™ IL-3 vial Additional cell vial |
Show product |
3-7 x 10e6 cells |
hkb-il3-av
|
![]() Cytokine offer: For each cytokine reporter cell line purchased, get a free vial of the matching cytokine.
Cytokine offer: For each cytokine reporter cell line purchased, get a free vial of the matching cytokine.
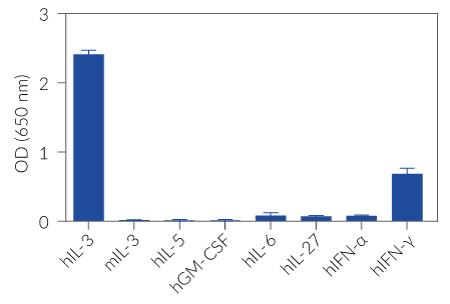
IL-3 responsive STAT5-SEAP reporter assay
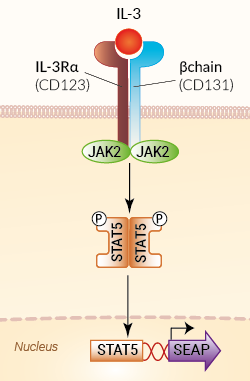
Signaling pathway in HEK-Blue™ IL-3 cells
InvivoGen also offers:
HEK-Blue™ IL-3 cells are designed to monitor human IL-3-induced STAT5 stimulation or inhibition. This colorimetric bioassay can be used for screening activatory molecules, such as engineered cytokines, or inhibitory molecules, such as neutralizing antibodies.
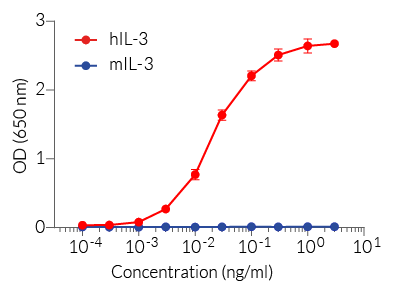
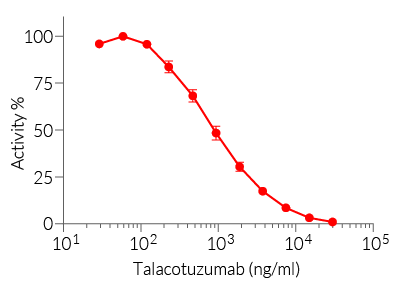
HEK-Blue™ IL-3 cells respond specifically to recombinant human IL-3. The reliable and consistent performance of HEK-Blue™ IL-3 cells makes them suitable for release assays of therapeutic molecules that inhibit IL-3 signaling, such as Talacotuzumab, a monoclonal antibody targeting the IL-3Rα chain of IL-3 receptor (see figures).
Key features
- Readily assessable STAT5-SEAP reporter activity
- Convenient readout using QUANTI-Blue™ Solution
- High sensitivity to human (h) IL-3 activity
- Stability guaranteed for 20 passages
Applications
- Therapeutic development
- Drug screening
- Release assay
Interleukin-3 (IL-3) is a cytokine that plays an important role in the recruitment, differentiation, and survival of a wide variety of hematopoietic cells, especially during inflammation. It is currently regarded as a regulator of inflammation with either protective or detrimental effects in the response to infections, immune-mediated diseases, and hematologic cancers.
All InvivoGen products are for internal research use only, and not for human or veterinary use.
Back to the topSpecifications
Cell type: Epithelial
Tissue origin: Human Embryonic Kidney
Target: IL-3
Specificity: Human
Reporter gene: SEAP
Antibiotic resistance: Blasticidin, Hygromycin, Zeocin®
Detection range: Human IL-3: 10 pg/ml -10 ng/ml
Growth medium: Complete DMEM (see TDS)
Growth properties: Adherent
Mycoplasma-free: Verified using Plasmotest™
Quality control: Each lot is functionally tested and validated.
Back to the topContents
HEK-Blue™ IL-3 Cells (hkb-il3)
- 1 vial containing 3-7 x 106 cells
- 1 ml of Blasticidin (10 mg/ml)
- 1 ml of Zeocin® (100 mg/ml)
- 1 ml of Normocin® (50 mg/ml)
-
1 ml of QB reagent and 1 ml of QB buffer (sufficient to prepare 100 ml of QUANTI-Blue™ Solution, a SEAP detection reagent)
HEK-Blue™ IL-3 vial (hkb-il3-av)
- 1 vial containing 3-7 x 106 cells
![]() Shipped on dry ice (Europe, USA, Canada and some areas in Asia)
Shipped on dry ice (Europe, USA, Canada and some areas in Asia)
Notification: Reference #hkb-il3-av can only be ordered together with reference #hkb-il3.
Back to the topDetails
Cell line description
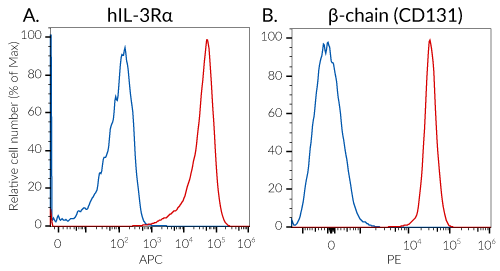
HEK-Blue™ IL-3 cells were generated by stable transfection of the human embryonic kidney HEK293 cell line with the gene encoding the human IL-3 receptor (IL-3Rα chain and common β-chain (CD131)) and STAT5 to obtain a fully active IL-3 signaling pathway. In addition, a STAT5-inducible secreted embryonic alkaline phosphatase (SEAP) reporter gene was introduced. The binding of IL-3 to its receptor triggers a signaling cascade leading to STAT5 activation and the subsequent production of SEAP. This can be readily assessed in the supernatant using QUANTI-Blue™ Solution, a SEAP detection reagent.
HEK-Blue™ IL-3 cells detect human (h) IL-3, but not mouse (m) IL-3. These cells also respond, to a weaker extent, to human IFN-γ. However, they do not respond to other STAT5-signaling cytokines of the common β-chain family: IL-5 and GMCSF (see figures).
IL-3 background
Interleukin-3 (IL-3) belongs to the common β chain (βc) cytokine family, originally identified as a multi-colony stimulation factor (CSF). It is now regarded as a regulator of inflammation [1, 2].
IL-3 expression is induced in response to inflammation, and is highly restricted to T cells. Under some circumstances, IL-3 may also be produced by macrophages, basophils, mast cells, NK cells and stromal cells [1, 3]. IL-3 binds a heterodimeric receptor comprising the βc (CD131) and IL-3Rα (CD123) subunits. It signals through tyrosine kinases of the Janus family (JAK2) and signal transducer and transcription activators (STATs), notably STAT5 [1, 3]. IL-3 supports the survival, proliferation, differentiation, polarization, or recruitment of immune and non-immune cells [2, 3]. Notably, as a multi-CSF, IL-3 targets a wide spectrum of hematopoietic cells, including eosinophils, basophils, plasmacytoid dendritic cells, neutrophils, and progenitor cells [3].
Relevance for therapeutics development
Depending on the clinical context, strategies have been investigated to either boost or disrupt IL-3 signaling [2, 3]. The administration of IL-3 has been evaluated as a treatment for patients with cytopenia (e.g. after chemotherapy). On the contrary, monoclonal antibodies or antibody-drug conjugates against IL-3Rα have been used in clinical trials to treat hematologic cancers. Indeed, the IL-3Rα subunit of the IL-3 receptor is overexpressed in acute myeloid lymphoma (AML), blastic plasmacytoid dendritic cell neoplasm (BPDCN), B-cell acute lymphoblastic leukemia, or Hodgkin lymphoma [2, 3].
Talacotuzumab (CSL362) is a monoclonal antibody targeting the IL-3Rα subunit, and exhibiting a modified Fc region for enhanced ADCC functions. Thus, it disrupts the IL-3 signaling and kills the malignant cells that overexpress IL-3Rα [4]. Although Talacotuzumab demonstrated promising activity in AML patients [5], later phase 2/3 clinical studies pointed to considerable toxicity [6].
References:
1. Dougan, M. et al., 2019. GM-CSF, IL-3, and IL-5 family of cytokines: regulators of inflammation. Immunity. 50(4):796-811.
2. Podolska, M.J. et al., 2024. IL-3: key orchestrator of inflammation. Front Immunol. 15:1411047.
3. Pant, H. et al., 2023. Translating the biology of β common receptor-engaging cytokines into clinical medicine. J. Allergy & Clin Immunol. 151(2):324-344.
4. Busfield, S.J. et al., 2014. Targeting of acute myeloid leukemia in vitro and in vivo with an anti-CD123 mAb engineered for optimal ADCC. Leukemia. 28(11):2213-2221.
5. Xie, L.H. et al., 2017. CD123 target validation and preclinical evaluation of ADCC activity of anti-CD123 antibody CSL362 in combination with NKs from AML patients in remission. Blood Cancer J 7(6):e567.
6. Montesinos P., et al., 2021. Safety and efficacy of talacotuzumab plus decitabine or decitabine alone in patients with acute myeloid leukemia not eligible for chemotherapy: results from a multicenter, randomized, phase 2/3 study. Leukemia 35, 62–74.